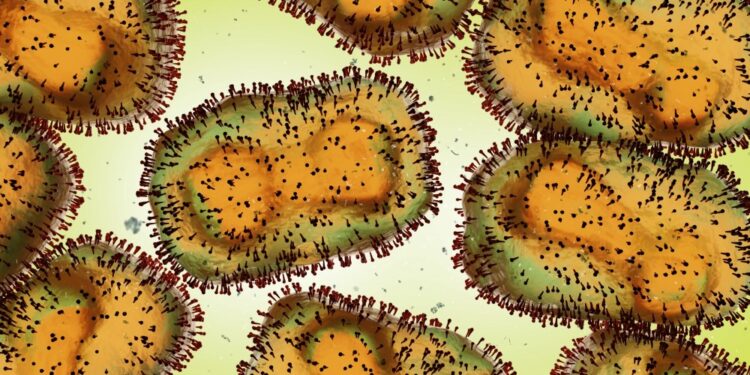
Mpox, formerly known as monkeypox, is an infectious disease caused by the mpox virus, a member of the Orthopoxvirus genus within the Poxviridae family. First identified in 1958 in laboratory monkeys, the virus was initially seen as a rare zoonotic disease primarily affecting regions in Central and West Africa. However, in recent years, global attention has turned towards mpox due to outbreaks occurring in non-endemic regions, highlighting its potential as an emerging global health threat. The understanding of mpox has evolved significantly, with a growing body of research shedding light on its transmission, clinical manifestations, and strategies for prevention and treatment.
Types of mpox
Mpox is classified into two distinct genetic clades based on the geographical regions where they are predominantly found:
1. West African clade
The West African clade is generally associated with a less severe form of the disease. This clade is typically characterized by lower mortality rates and less frequent human-to-human transmission. The outbreaks associated with this clade have predominantly occurred in West African countries, such as Nigeria, Sierra Leone, and Liberia. However, cases have also been reported in non-endemic regions, particularly during the 2022 global outbreak.
2. Central African (Congo Basin) clade
The Central African clade, found mainly in the Congo Basin, is considered more virulent and transmissible. This clade is associated with higher mortality rates and more severe clinical presentations, including complications such as encephalitis. Human-to-human transmission is more common with this clade, often resulting in larger outbreaks in affected communities.
Causes of mpox
Mpox is caused by the mpox virus, an enveloped double-stranded DNA virus belonging to the Orthopoxvirus genus. The Orthopoxvirus genus also includes other notable viruses, such as variola (which causes smallpox), vaccinia (used in the smallpox vaccine), and cowpox viruses.
1. Zoonotic transmission
The primary mode of transmission of mpox is zoonotic, meaning it is transmitted from animals to humans. The natural reservoir of the mpox virus is not definitively known, but evidence suggests that rodents, particularly African squirrels, dormice, and Gambian pouched rats, may be the primary hosts. Monkeys and other non-human primates are also susceptible to the virus but are considered incidental hosts rather than reservoirs. Humans can acquire the virus through direct contact with the blood, bodily fluids, or cutaneous or mucosal lesions of infected animals. Activities such as hunting, handling, or consuming bushmeat in endemic regions increase the risk of zoonotic transmission.
2. Human-to-human transmission
Human-to-human transmission occurs primarily through close contact with respiratory secretions, skin lesions, or contaminated objects (fomites) such as bedding or clothing. The virus can also be transmitted through respiratory droplets during prolonged face-to-face contact. However, unlike diseases like COVID-19, the mpox virus is not as easily transmissible through respiratory routes alone. Sexual transmission has emerged as a significant mode of transmission during recent outbreaks, particularly among men who have sex with men (MSM). The presence of the virus in genital and rectal swabs has raised concerns about its potential as a sexually transmitted infection (STI).
Symptoms of mpox
The clinical presentation of mpox varies depending on the clade of the virus and the individual’s immune response. The disease generally presents with a range of symptoms that can be grouped into the following categories:
1. Prodromal symptoms
The prodromal phase of mpox typically begins 5 to 21 days after exposure and lasts for 1 to 5 days. During this phase, patients may experience:
- Fever: A sudden onset of high fever (often above 38.3°C or 101°F) is common.
- Headache: Intense headaches are frequently reported.
- Lymphadenopathy: Swelling of lymph nodes, particularly in the neck, armpits, and groin, is a distinctive feature of mpox that helps differentiate it from other pox-like diseases such as smallpox.
- Myalgia: Muscle aches and pains are common.
- Fatigue: Generalized weakness and fatigue often accompany other symptoms.
2. Skin rash
Following the prodromal phase, a characteristic rash appears, usually starting on the face and then spreading to other parts of the body, including the palms and soles. The rash progresses through several stages:
- Macules: Flat, red spots appear on the skin, typically beginning on the face.
- Papules: The macules evolve into raised lesions known as papules.
- Vesicles: The papules then fill with clear fluid, forming vesicles.
- Pustules: The vesicles become filled with pus, resulting in pustules. This stage is often the most uncomfortable, as the pustules can be itchy and painful.
- Scabs: The pustules eventually dry up and form scabs, which later fall off, sometimes leaving scars.
3. Systemic symptoms
In addition to the rash, patients may experience systemic symptoms such as:
- Chills and sweats: Alternating episodes of chills and sweating are common.
- Backache: Severe back pain, particularly in the lower back, is often reported.
- Sore throat and cough: Respiratory symptoms such as sore throat and cough may occur, especially in cases with respiratory droplet transmission.
Stages of mpox
The progression of mpox can be divided into several stages, each characterized by specific clinical features:
1. Incubation period
The incubation period, lasting 5 to 21 days, is the time between exposure to the virus and the onset of symptoms. During this period, the virus multiplies in the body without causing noticeable symptoms.
2. Prodromal stage
The prodromal stage, lasting 1 to 5 days, is marked by the onset of non-specific symptoms such as fever, headache, and lymphadenopathy. These symptoms indicate the initial immune response to the virus.
3. Eruptive stage
The eruptive stage begins with the appearance of the characteristic rash, which progresses through macular, papular, vesicular, and pustular stages over 2 to 4 weeks. This stage is the most visible and often the most uncomfortable.
4. Recovery stage
The recovery stage is marked by the resolution of the rash as the pustules dry up and scab over. This stage can last several weeks, and while most patients recover without complications, some may develop secondary bacterial infections or scarring.
Prevention of mpox
Preventing mpox involves a combination of strategies, including vaccination, public health measures, and individual precautions.
1. Vaccination
The smallpox vaccine, which contains live vaccinia virus, provides cross-protection against mpox due to the genetic similarities between the two viruses. In countries where smallpox vaccination was routine, it provided significant protection against mpox, though the global cessation of smallpox vaccination programs in the 1980s has led to a decline in immunity levels. In response to mpox outbreaks, the use of newer vaccines such as Modified Vaccinia Ankara (MVA) has been recommended. MVA is a third-generation vaccine that is considered safer than earlier vaccines and is licensed for both smallpox and mpox prevention.
2. Public health measures
Public health strategies to prevent mpox include:
- Surveillance: Monitoring and reporting cases in both endemic and non-endemic regions is crucial for early detection and response.
- Isolation: Infected individuals should be isolated to prevent transmission to others. Healthcare workers should use appropriate personal protective equipment (PPE) when caring for patients.
- Contact tracing: Identifying and monitoring individuals who have been in close contact with infected persons can help prevent the spread of the virus.
3. Individual precautions
Individuals can reduce their risk of mpox by:
- Avoiding contact with wild animals: In endemic regions, avoiding contact with rodents and primates, and refraining from consuming bushmeat, can reduce the risk of zoonotic transmission.
- Practicing good hygiene: Regular handwashing and maintaining good personal hygiene can help prevent the spread of the virus.
- Using barrier protection during sex: Given the emerging evidence of sexual transmission, using condoms and engaging in safer sex practices can reduce the risk of infection.
Diagnosis of mpox
Diagnosing mpox involves a combination of clinical evaluation, laboratory testing, and differential diagnosis to rule out other diseases with similar presentations.
1. Clinical evaluation
The characteristic rash, particularly the progression from macules to pustules, is a key clinical feature that aids in the diagnosis of mpox. Lymphadenopathy, which is not typically seen in other poxvirus infections, is another important clinical clue.
2. Laboratory testing
Laboratory confirmation of mpox is essential for a definitive diagnosis. The following tests are commonly used:
- Polymerase Chain Reaction (PCR): PCR is the most reliable method for detecting mpox virus DNA in clinical samples, such as swabs from skin lesions. It is highly specific and can differentiate between different Orthopoxviruses.
- Serology: Serological tests can detect antibodies against the mpox virus, but they are less useful for diagnosing acute infections, as antibodies may not be present in the early stages of the disease.
- Viral culture: While viral culture can isolate the mpox virus, it is less commonly used due to its complexity and the availability of more rapid and specific tests.
3. Differential diagnosis
Mpox shares clinical features with several other diseases, making differential diagnosis important. Conditions to consider include:
- Chickenpox (Varicella): Chickenpox presents with a similar vesicular rash but typically lacks the prominent lymphadenopathy seen in mpox.
- Smallpox: Although eradicated, smallpox is a key differential due to its similar rash. The presence of lymphadenopathy and the more rapid progression of mpox lesions help distinguish the two.
- Measles: Measles can cause a maculopapular rash, but the presence of Koplik spots and a history of exposure to an infected individual can help differentiate it from mpox.
Treatment of mpox
There is no specific antiviral treatment approved for mpox, but supportive care and certain antiviral agents can help manage symptoms and reduce complications.
1. Supportive care
Supportive care is the cornerstone of mpox treatment and includes:
- Pain management: Analgesics such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) can help alleviate pain and fever.
- Hydration: Ensuring adequate hydration is important, especially in patients with severe systemic symptoms or gastrointestinal involvement.
- Skin care: Proper wound care is essential to prevent secondary bacterial infections of the skin lesions. Topical antiseptics or antibiotics may be used if necessary.
2. Antiviral agents
While no antiviral agents are specifically approved for mpox, some drugs have shown efficacy in laboratory and clinical settings:
- Tecovirimat (TPOXX): Tecovirimat is an antiviral agent approved for the treatment of smallpox but has shown promise in treating mpox as well. It works by inhibiting the viral envelope protein, preventing the release of the virus from infected cells.
- Cidofovir: Cidofovir, an antiviral used to treat cytomegalovirus (CMV) infections, has demonstrated activity against poxviruses in laboratory studies. However, its use is limited by potential nephrotoxicity.
- Brincidofovir: Brincidofovir, a lipid-conjugated form of cidofovir, has a better safety profile and has been considered for use in treating mpox, particularly in severe cases or in immunocompromised patients.
3. Vaccination post-exposure
In certain cases, vaccination with the smallpox vaccine may be considered for individuals who have been exposed to the mpox virus. Post-exposure prophylaxis (PEP) with the smallpox vaccine can reduce the severity of the disease if administered within 4 days of exposure.
Conclusion
Mpox is a complex and evolving infectious disease with significant implications for global public health. Its zoonotic origins, potential for human-to-human transmission, and varying clinical presentations underscore the importance of comprehensive prevention, diagnosis, and treatment strategies. As the global health community continues to grapple with the challenges posed by emerging infectious diseases, the lessons learned from mpox will undoubtedly inform future efforts to combat similar threats. Continued research, public health vigilance, and international cooperation will be crucial in mitigating the impact of mpox and ensuring that the world is better prepared for future outbreaks.